Shin pain is a common complaint of soccer players especially early in the season or with significant increase in activity during the course of the season. I see it with my players when we transition from training on turf to playing futsal in a gym to mix it up in the winter months. I also see it in players who are playing multiple sports with overlapping seasons.
The term “shin splints” is often the term that gets thrown around for any type of shin pain that isn’t a result of direct trauma to the leg. It’s really used as a generic term in much the same manner that anterior knee pain, tendonitis, and low back pain are used to describe regional aches and pains.
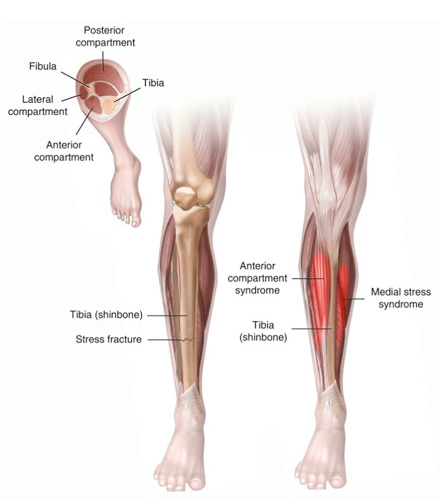
Medial Tibial Stress Syndrome
WHAT IS HAPPENING:
There are a number of muscles in the lower leg that attach to the two bones, tibia (shin) and fibula, of the lower leg. When these muscles get overworked and fatigued while trying to provide stability to the ankle and foot they can become inefficient in providing shock absorption to the lower leg. This can set the stage for a stress fracture OR tendons can starting to pull away from the bone itself and inflame the outer cover (periosteum) of the bone. This is especially seen with the tibial attachments of the soleus and posterior tibialis muscles of the lower leg.
SYMPTOMS:
Pain on the inside lower part of the tibia (shin bone)
Pain with activity; may be at its worst the next morning
May experience swelling
Pain with pointing toes downward
WHAT CAUSES IT:
1. Overuse – too much overall activity or ramping up activity too quickly, especially on uneven and/or hard surfaces
2. Biomechanics – altered foot, knee, and hip posture; especially flat feet and over pronation. The posterior tibialis has to work extra hard in controlling the fall of the arch and transfer of force toward the medial (big toe) side of the foot with weight bearing and thus can become fatigued or create traction forces on the tibia. In addition, other muscles become overstretched from the rolling/twisting of the foot inward.
3. Tight/stiff lower leg muscles
4. Worn out or ill-fitting shoes
HOW TO TREAT:
1. Rest / Time off – especially if symptoms appear in the middle of the season
2. Gradual Increase in Training Activity – at the beginning of seasons and when on new surfaces
3. Ice after activity to control inflammation
4. Compression after initial/acute stage to promote blood flow and healing; Compression sleeve as needed before activity and during activity to provide support for muscles/tendons
5. Stretch muscles of lower leg, especially calf muscles and posterior tibialis
6. Strengthen small muscles of foot that provide arch and stability (yes, that is something you can improve)
7. Biomechanical assessment – gait analysis, posture
8. If pain persists, becomes worse, or is accompanied by numbness/tingling – follow-up with sports medicine professional to rule out development of stress fracture and/or compartment syndrome
Tibial Stress Fractures
WHAT IS HAPPENING:
A bone is an active substance that adapts to the stresses which are placed upon it; this is known as Wolff’s Law. When a bone experiences repetitive stress, a temporary weakening of the bone will result. With adequate rest, new bone will form and reinforce overall strength of the bone (which is why weight-bearing activity is good for the prevention of osteoporosis). If there is inadequate rest, stress fractures can occur because the frequency of micro trauma/weakening exceeds the rate of bone remodeling. Then you have a problem.
SYMPTOMS:
Pain in lower 1/3 of the tibia (shin bone) most often, but not always
Pain with weight bearing activities – especially running and hopping
Tenderness and swelling of lower leg – usually becoming more focal as fracture worsens
WHAT CAUSES IT:
1. Overload – continuous contraction of muscles with repetitive movement (running/cutting) and fatigued muscles leading to poor shock absorption
2. Biomechanics – altered foot, knee, and hip posture leading to inefficient movement and poor force absorption
3. Poor Bone Mineral Density / Nutrition – phosphates from soda leech calcium from the bones and a daily soda increases your risk of stress fractures by 3-4 times
4. Amenorrhea increases risk of stress fracture in female runners by 4.5 times
5. Poor shoes – especially if coupled with overload and poor biomechanics

HOW TO TREAT:
1. See Sports Medicine physician or orthopedist for evaluation – stress fractures often do not show up on X-rays in the early stages and can take up to 4 weeks to appear. Stress fractures can become complete fractures of the bone if not treated properly. Your doctor will be able to advise appropriately.
2. Rest / Time Off – in some cases limits on weight bearing on affected leg
3. Use of non-weight bearing activities (swimming/biking) to maintain cardiovascular fitness
4. Proper nutrition to promote healthy bone growth (no soda, get adequate daily intake of calcium and vitamin D). Bones take 6-8 weeks to heal, generally.
Next Article: Lateral Ankle Sprains – how to treat effectively, how to prevent them.
Want a soccer injury topic addressed? Feel free to send in requests!
About the Author: Julie Eibensteiner PT, DPT, CSCS is a physical therapist and owner of Laurus Athletic Rehab and Performance LLC, an independently owned practice specializing in ACL rehab and prevention in competitive athletes. In addition to being a regular contributor to IMS on topics of sport injury and prevention, Eibensteiner holds an USSF A License, coaches a U18G MRL team for Eden Prairie Soccer Club, and assists with the Men’s and Women’s soccer programs at Macalester College.
To view other sports injury and rehab articles by Julie Eibensteiner click here.

 Clap
Clap